Diabetes and Vascular Disease: Understanding the Connection and Taking Control
Diabetes is a chronic condition that affects millions of people worldwide. While most individuals are aware of the impact of diabetes on blood sugar control, many may not fully understand the profound effect it can have on the vascular system. Diabetes significantly increases the risk of developing various vascular diseases, emphasizing the importance of managing the condition effectively. Let’s delve into the connection between diabetes and vascular disease and explore strategies to minimize its impact.
Understanding the Link:
Diabetes is characterized by elevated blood glucose levels, which can damage blood vessels over time. The persistently high levels of glucose in the bloodstream can lead to the accumulation of fatty deposits in the vessel walls, causing a condition called atherosclerosis. Atherosclerosis is a significant contributor to various vascular diseases, including:
Peripheral Artery Disease (PAD):
Diabetes increases the risk of developing PAD, which affects the blood vessels supplying the legs and feet. Reduced blood flow to the lower extremities can result in pain, slow wound healing, and an increased risk of infections and amputations.
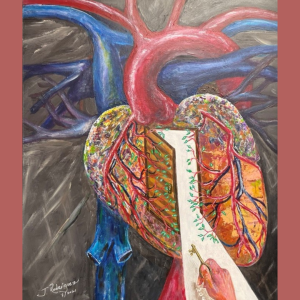
Coronary Artery Disease (CAD):
Individuals with diabetes are more prone to CAD, a condition that affects the blood vessels supplying the heart. Narrowed or blocked arteries can lead to chest pain (angina), heart attacks, and other cardiovascular complications.
Stroke:
Diabetes raises the risk of stroke by accelerating the development of atherosclerosis in the arteries supplying the brain. A clot or rupture in these arteries can result in a stroke, causing lasting damage or even death.
Diabetic Retinopathy:
The blood vessels in the retina can be damaged by diabetes, leading to diabetic retinopathy. This condition can cause vision loss or even blindness if left untreated.
Diabetic Nephropathy:
High blood glucose levels can impair the kidneys’ ability to filter waste products, leading to diabetic nephropathy. It is a progressive kidney disease that can eventually result in kidney failure.
Managing Diabetes and Vascular Disease:
While the connection between diabetes and vascular disease may seem daunting, it’s important to remember that taking proactive steps can significantly reduce the risks. Here are some strategies to manage diabetes and minimize the impact on the vascular system:
Maintain Blood Sugar Levels:
Consistently monitoring and managing blood sugar levels through a healthy diet, regular exercise, and appropriate medication or insulin therapy is crucial. Keeping blood glucose within target ranges helps minimize damage to blood vessels.
Control Blood Pressure and Cholesterol:
High blood pressure and elevated cholesterol levels further contribute to vascular disease. Regular monitoring and effective management of these factors through lifestyle modifications and medications are essential.
Adopt a Healthy Lifestyle:
Engage in regular physical activity, such as walking, swimming, or cycling, to improve circulation and maintain a healthy weight. Follow a balanced diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats while limiting sugary and processed foods.
Quit Smoking:
Smoking damages blood vessels and significantly increases the risk of vascular disease. Quitting smoking is one of the most beneficial steps individuals with diabetes can take to protect their vascular health.
Regular Check-ups:
Maintain regular check-ups with healthcare professionals to monitor blood sugar control, blood pressure, cholesterol levels, and overall vascular health. Early detection and intervention can prevent or minimize the progression of vascular diseases.
Diabetes and vascular disease are intricately linked, underscoring the importance of proactive management. By effectively managing blood sugar levels, controlling blood pressure and cholesterol, adopting a healthy lifestyle, and seeking regular medical care, individuals with diabetes can significantly reduce their risk of developing or worsening vascular disease. Empower yourself with knowledge, take control of your diabetes, and prioritize your vascular health for a better quality of life.